pathophysiology of congestive heart failure pdf
Dive deep into the pathophysiology of congestive heart failure with our comprehensive PDF guide. Uncover the complex mechanisms, learn about the stages, and gain valuable insights into this critical condition. Download now for free!
Pathophysiology of Congestive Heart Failure
Congestive heart failure (CHF) arises from structural or functional impairments hindering ventricular filling or blood ejection, thus failing to meet the body’s circulatory demands. It’s a complex syndrome stemming from various cardiac abnormalities, impacting structure, function, rhythm, or a combination thereof. The resulting hemodynamic changes trigger compensatory mechanisms, which, if unchecked, lead to maladaptive remodeling and disease progression.
Definition and Epidemiology of Congestive Heart Failure
Congestive heart failure (CHF), also known as heart failure, is a clinical syndrome defined by the heart’s inability to effectively pump blood to meet the body’s metabolic needs. This inadequacy can stem from structural or functional issues within the heart, impacting either the filling of the ventricles with blood or the ejection of blood into the systemic circulation. The prevalence of CHF is substantial, affecting a significant portion of the global population. The exact figures vary depending on the criteria used for diagnosis and the population studied. However, it’s widely recognized as a major public health concern, contributing significantly to morbidity and mortality worldwide. Risk factors are numerous and complex, encompassing both modifiable and non-modifiable elements. Understanding the definition and epidemiological aspects is crucial for effective prevention and management strategies.
Etiology and Risk Factors of Congestive Heart Failure
The etiology of congestive heart failure (CHF) is multifaceted, with a range of contributing factors often interacting to initiate and exacerbate the condition. Coronary artery disease, a leading cause, restricts blood flow to the heart muscle, weakening its pumping ability. Hypertension, by increasing the workload on the heart, can lead to progressive weakening. Valvular heart disease, where heart valves malfunction, disrupts the normal flow of blood, placing strain on the heart. Inherent myocardial diseases, such as cardiomyopathies, directly impair the heart muscle’s contractile function. Additionally, conditions like diabetes and chronic kidney disease contribute significantly to the development of CHF. Lifestyle factors, including smoking, obesity, and physical inactivity, further increase the risk. While some risk factors are non-modifiable, such as age and family history, others can be managed through lifestyle changes and medical interventions to mitigate the risk of developing CHF.
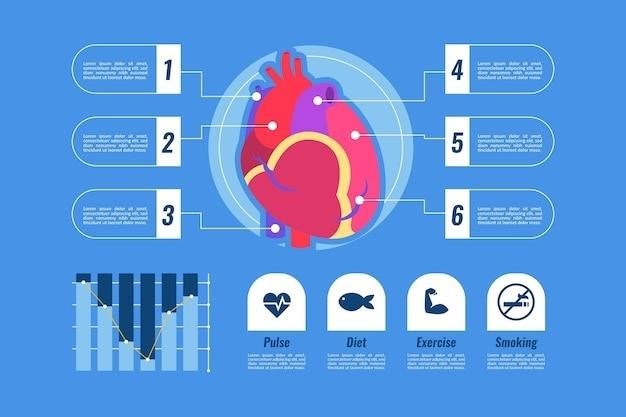
Hemodynamic Abnormalities in Congestive Heart Failure
The hallmark of congestive heart failure (CHF) lies in its characteristic hemodynamic disturbances. Reduced cardiac output, the volume of blood pumped by the heart per minute, is a central feature. This decrease stems from impaired myocardial contractility, leading to insufficient ejection of blood into the systemic circulation. Simultaneously, elevated filling pressures within the heart chambers, particularly the left ventricle, arise due to the heart’s inability to efficiently handle the returning venous blood. This increase in pressure is reflected in elevated pulmonary capillary wedge pressure, indicative of congestion in the pulmonary circulation. Systemic venous pressures also rise, resulting in peripheral edema. The reduced cardiac output, coupled with increased filling pressures, creates a vicious cycle. The body’s compensatory mechanisms, while initially beneficial, ultimately contribute to further hemodynamic instability and disease progression. Understanding these hemodynamic abnormalities is crucial for diagnosing and managing CHF effectively.
Compensatory Mechanisms and Maladaptive Remodeling
Initially, the body attempts to compensate for reduced cardiac output through neurohormonal activation and structural changes. However, these adaptations become maladaptive, worsening the condition and leading to progressive heart failure.
Neurohormonal Activation in Congestive Heart Failure
In response to decreased cardiac output and tissue perfusion, the neurohormonal system is activated. The renin-angiotensin-aldosterone system (RAAS) plays a crucial role, with renin release leading to angiotensin II production. Angiotensin II is a potent vasoconstrictor, increasing systemic vascular resistance and blood pressure, attempting to maintain perfusion. Aldosterone, stimulated by angiotensin II, promotes sodium and water retention, increasing blood volume and further elevating pressure. However, these effects are ultimately detrimental. The sustained vasoconstriction increases afterload, stressing the already weakened heart. Fluid retention exacerbates pulmonary and systemic congestion, worsening symptoms. Sympathetic nervous system activation also contributes, releasing catecholamines (epinephrine and norepinephrine). These increase heart rate and contractility, providing a short-term boost but accelerating myocardial damage over time due to increased oxygen demand and potential arrhythmias. The chronic activation of the RAAS and sympathetic nervous system contributes significantly to the progression of heart failure.
Structural and Functional Cardiac Remodeling
Persistent neurohormonal activation and hemodynamic stress in congestive heart failure induce significant structural and functional changes within the heart. Left ventricular hypertrophy, an increase in the size of the heart muscle cells, is a common response to increased workload. Initially, this compensates for reduced contractility, but eventually leads to impaired diastolic function, reducing the heart’s ability to relax and fill efficiently. Myocardial fibrosis, the replacement of healthy heart muscle tissue with scar tissue, further impairs contractility and contributes to electrical instability, increasing the risk of arrhythmias. These structural changes are accompanied by alterations in intracellular calcium handling, impacting the force and timing of muscle contractions. The heart becomes less efficient at pumping blood, and the capacity for normal function progressively diminishes. Remodeling also extends to the other heart chambers, potentially leading to right ventricular dysfunction, further complicating the clinical picture. This vicious cycle of neurohormonal activation, hemodynamic stress, and maladaptive remodeling drives the relentless progression of congestive heart failure.
Clinical Manifestations and Staging of Congestive Heart Failure
Clinical presentation varies widely, depending on disease severity and the affected chambers. Symptoms range from subtle fatigue and shortness of breath to severe dyspnea and edema. Staging systems categorize disease progression, guiding treatment strategies and predicting prognosis.
Symptoms and Signs of Congestive Heart Failure
The clinical presentation of congestive heart failure (CHF) is diverse, reflecting the complex interplay of hemodynamic derangements and compensatory mechanisms. Common symptoms include exertional dyspnea (shortness of breath with exertion), orthopnea (shortness of breath when lying flat), paroxysmal nocturnal dyspnea (sudden shortness of breath at night), and persistent cough, often productive of frothy sputum. Fatigue and reduced exercise tolerance are frequently reported, reflecting the diminished cardiac output. Physical examination may reveal elevated jugular venous pressure (JVP), indicating right-sided heart failure, and pulmonary rales (crackles), signifying fluid accumulation in the lungs. Peripheral edema, particularly in the lower extremities, is a common finding, reflecting increased capillary hydrostatic pressure. Other signs include hepatomegaly (enlarged liver) and ascites (abdominal fluid accumulation) due to systemic venous congestion. In advanced cases, patients may experience cyanosis (bluish discoloration of the skin and mucous membranes) due to impaired oxygenation. The severity and combination of these symptoms and signs vary considerably among individuals, making accurate assessment crucial for effective management.
Classification and Staging of Congestive Heart Failure
Congestive heart failure (CHF) classification systems aim to stratify patients based on disease severity and prognosis, guiding treatment decisions. The New York Heart Association (NYHA) functional classification categorizes patients into four classes (I-IV) based on the limitation of physical activity imposed by symptoms. Class I patients are asymptomatic, while Class IV patients experience symptoms even at rest. The American College of Cardiology (ACC) and American Heart Association (AHA) staging system provides a more comprehensive approach, incorporating symptoms, structural and functional parameters, and risk factors. Stage A identifies individuals at high risk of developing CHF but without structural heart disease. Stages B, C, and D represent increasing levels of disease severity and symptoms. Stage B includes patients with structural heart disease but without symptoms. Stage C involves patients with prior or current symptoms of CHF. Stage D signifies refractory CHF requiring advanced therapies like transplantation or mechanical circulatory support. These classifications assist in risk stratification, treatment planning, and monitoring disease progression. Accurate staging is crucial for optimizing patient care and improving outcomes.