single leg stance test pdf
Improve your balance and stability with this easy-to-follow single leg stance test PDF. Download now and get started!
The Single Leg Stance (SLS) Test
The Single Leg Stance (SLS) Test is used to assess static postural and balance control. Abnormal values may indicate conditions such as peripheral neuropathy, … The timed unipedal stance test (also referred to as timed single limb stance, unipedal balance test, one leg stance test, and one-leg standing balance) is a … The single leg stance test measures a persons ability to balance on one leg. To perform the test, the person stands on one leg with hands on hips while being …
Introduction
The Single Leg Stance (SLS) Test, also known as the timed unipedal stance test, is a widely used clinical assessment tool that measures an individual’s ability to maintain balance on one leg. This test is a simple yet effective measure of static postural control and balance, which are crucial components of overall functional mobility and independence. The SLS Test is commonly employed in various healthcare settings, including physical therapy, neurology, and geriatrics, to evaluate balance deficits, monitor treatment progress, and assess fall risk.
The SLS Test is a valuable tool for assessing balance impairments in a variety of conditions, including stroke, Parkinson’s disease, multiple sclerosis, and peripheral neuropathy. It is also useful in evaluating balance deficits associated with aging, musculoskeletal injuries, and vestibular disorders. The test is particularly relevant in identifying individuals at risk for falls, a significant public health concern, especially among older adults.
The SLS Test is typically performed with the individual standing on one leg with their eyes open or closed, depending on the specific protocol. The time the individual can maintain the stance without losing balance is recorded. The simplicity of the test makes it readily adaptable to various clinical settings and allows for efficient assessment of balance capabilities.
Purpose of the Test
The Single Leg Stance (SLS) Test serves a multifaceted purpose in clinical practice, providing valuable insights into an individual’s balance capabilities and potential risk factors. Primarily, the SLS Test aims to assess static postural control, which refers to the ability to maintain a stable body position against gravity while standing on one leg. This assessment is crucial for understanding an individual’s ability to maintain balance and stability during everyday activities, such as walking, turning, and reaching.
Beyond assessing static postural control, the SLS Test can also be used to identify individuals at risk for falls. Studies have shown a strong correlation between poor performance on the SLS Test and an increased likelihood of experiencing falls. The test’s ability to detect subtle balance impairments can be instrumental in implementing preventive measures and tailoring interventions to reduce fall risk.
Moreover, the SLS Test serves as a valuable tool for monitoring treatment progress and evaluating the effectiveness of interventions aimed at improving balance and reducing fall risk. By comparing scores over time, healthcare professionals can track improvements in balance and adjust treatment strategies as needed. The test’s simplicity and ease of administration make it an efficient and effective tool for monitoring balance function over time.
Method
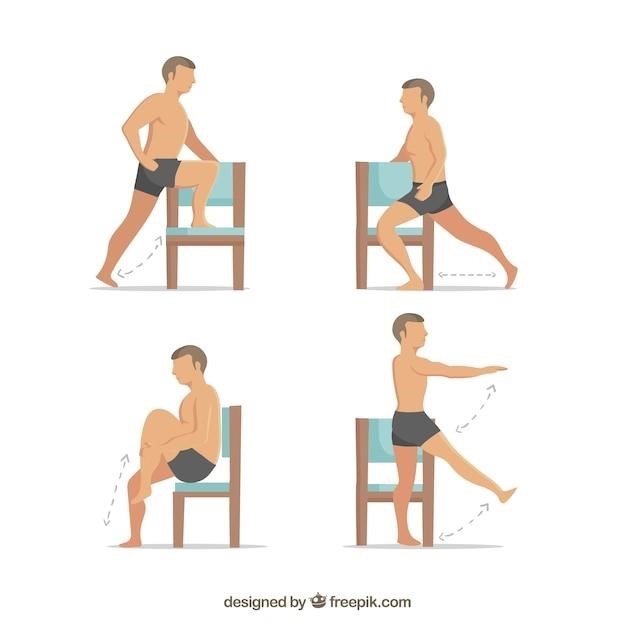
The Single Leg Stance (SLS) Test is a straightforward procedure that can be performed with minimal equipment. To execute the test, the individual stands on one leg with their arms crossed at chest level, ensuring their hands touch their shoulders. For safety reasons, it is generally recommended to conduct the test with eyes open only. A stopwatch is used to measure the duration of time the individual can maintain the single-leg stance without losing balance or making any movement errors.
To ensure consistency and accuracy, several parameters are typically defined for the test. These include⁚
- Starting Position⁚ The individual should stand on one leg with their arms crossed at chest level, and their hands should touch their shoulders.
- Eyes Open⁚ It is generally recommended to conduct the test with eyes open only.
- Movement Errors⁚ Errors that may result in termination of the test include the following⁚
- The legs touching each other
- The feet moving on the floor
- The foot touching down
- The eyes opening during the eyes closed test
- The arms moving from their start position
The SLS Test can be performed with either the dominant or non-dominant leg, depending on the specific purpose of the assessment. It is common to perform the test on both legs to compare balance performance between sides.
Clinical Implications
The Single Leg Stance (SLS) Test holds significant clinical implications, particularly in the assessment and management of balance disorders, neurological conditions, and musculoskeletal injuries. The test provides valuable insights into an individual’s static postural control and balance capabilities, which can be crucial for identifying potential fall risks and guiding rehabilitation strategies.
For instance, the SLS Test has been widely employed in the assessment of patients with Parkinson’s Disease (PD). Research has demonstrated a strong correlation between impaired balance, as measured by the SLS Test, and an increased risk of falls in individuals with PD. This information is critical for healthcare professionals to develop personalized interventions aimed at improving balance and reducing fall incidence in this population.
Furthermore, the SLS Test has proven useful in evaluating balance recovery following a stroke. By monitoring changes in SLS test performance over time, clinicians can track a patient’s progress during rehabilitation and tailor therapy programs to address specific balance impairments.
Beyond neurological conditions, the SLS Test can also be applied to assess balance deficits associated with musculoskeletal injuries, such as ankle sprains or knee replacements. The test can help identify individuals who may benefit from balance-specific exercises to restore stability and reduce the risk of re-injury.
Evidence
The validity and reliability of the Single Leg Stance (SLS) Test as a measure of balance and postural control have been extensively studied, providing robust evidence for its clinical utility. Numerous research studies have demonstrated a strong correlation between SLS performance and fall risk, particularly in older adults and individuals with neurological conditions such as Parkinson’s Disease (PD).
A meta-analysis of 10 studies, published in the journal “Gait & Posture” in 2011, concluded that the SLS Test, with eyes open, is a reliable and valid measure of balance in healthy older adults. The meta-analysis found that SLS times of approximately 10 seconds or less were associated with an increased risk of falls, highlighting the test’s potential for identifying individuals at higher risk.
Similarly, a study published in the journal “Movement Disorders” in 2012 demonstrated the predictive value of the SLS Test for falls in individuals with PD. The study found that a cut-off score of 10 seconds on the SLS Test provided good sensitivity and specificity for predicting fall history in this population.
Further research has investigated the use of the SLS Test in other clinical settings, including stroke rehabilitation and the assessment of balance deficits following musculoskeletal injuries. These studies have generally supported the reliability and validity of the SLS Test for these applications, further solidifying its role as a valuable tool for clinicians.
Variations of the Test
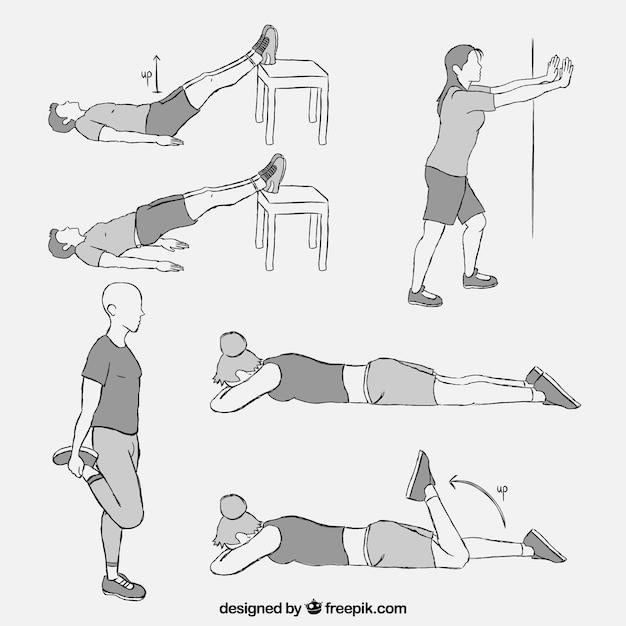
The Single Leg Stance (SLS) Test can be modified to increase its challenge and assess different aspects of balance control. These variations allow clinicians to tailor the test to the specific needs of the individual being assessed and to gather more comprehensive information about their balance capabilities.
One common variation involves altering the visual input by having the patient perform the test with their eyes closed. This modification increases the difficulty of the test, as it eliminates the visual feedback that helps with maintaining balance. Another variation involves adding a cognitive challenge, such as having the patient count backwards from 100 or recite the alphabet. This variation assesses the ability to maintain balance while performing a mentally demanding task.
Additionally, the position of the arms can be varied. The standard protocol requires the patient to keep their arms crossed across their chest. However, the arms can be raised overhead, placed on the hips, or kept at the sides. These variations can influence the stability of the body and provide insights into the role of upper body movement in balance control.
Furthermore, the surface on which the test is performed can be altered. The standard protocol involves performing the test on a firm, level surface. However, the test can also be performed on a soft surface, such as a foam mat, or on an unstable surface, such as a balance board. These variations can assess the ability to maintain balance under different conditions and provide information about the individual’s adaptability and postural control.
Interpretation of Results
The interpretation of the SLS test results is crucial for understanding the patient’s balance capabilities and identifying potential risk factors for falls. Several factors contribute to the interpretation, including the time the patient is able to maintain the single-leg stance, the presence or absence of errors during the test, and the individual’s age, health condition, and physical activity level.
A shorter stance time generally indicates poorer balance control and a higher risk of falls. However, it’s important to consider the individual’s baseline performance and the specific variations of the test that were used. For example, a shorter stance time with eyes closed might be expected compared to a stance time with eyes open, indicating a greater reliance on visual feedback for balance control.
Errors during the test, such as the leg touching the ground, the body swaying excessively, or the arms moving from their starting position, also provide valuable information. These errors can suggest impairments in specific aspects of balance control, such as proprioception, vestibular function, or motor control.
Normative data is also important for interpreting the results. While there are no universally accepted norms for the SLS test, studies have established average stance times for different age groups and health conditions. Comparing the patient’s results to these normative values can help determine whether their performance is within an expected range or falls outside the typical range, suggesting a possible balance impairment.
Normative Data
Establishing normative data for the Single Leg Stance (SLS) test is crucial for interpreting individual results and identifying potential balance impairments. While there is no universally accepted standard, several studies have investigated SLS performance in healthy individuals, providing valuable insights into expected values for different age groups and conditions.
For instance, a meta-analysis examining SLS times with eyes open in healthy elderly individuals found that the mean times for different age groups were 27.0, 17.2, and 8.5 seconds, respectively. These findings suggest that SLS performance decreases with age, highlighting the importance of considering age-related variations when interpreting results.
Furthermore, studies have shown that individuals with specific health conditions, such as Parkinson’s disease (PD) or stroke, often exhibit shorter SLS times compared to healthy controls. Understanding these differences in performance is essential for identifying individuals at higher risk of falls and for guiding interventions aimed at improving balance control.
It’s important to note that normative data can vary depending on the specific test protocol, including the instructions given to participants, the presence or absence of visual cues, and the criteria for errors. Therefore, when interpreting individual results, it’s crucial to compare them to normative data derived from studies using similar methodologies.
Factors Affecting Performance
Several factors can influence an individual’s performance on the Single Leg Stance (SLS) test, impacting their ability to maintain balance and stand on one leg for an extended period. Understanding these factors is essential for interpreting test results and identifying potential underlying impairments.
Age is a significant factor, with older individuals typically demonstrating shorter SLS times compared to younger adults. This decline in balance control is often attributed to age-related changes in muscle strength, proprioception, and sensory processing.
Sensory input plays a crucial role in maintaining balance. Visual cues, such as a fixed point to focus on or the presence of obstacles, can influence SLS performance. Similarly, proprioception, the body’s awareness of its position in space, is essential for postural stability. Impairments in these sensory systems can lead to difficulty maintaining balance during the SLS test.
Neurological conditions, such as Parkinson’s disease, stroke, and peripheral neuropathy, can significantly impact balance control and SLS performance. These conditions often result in muscle weakness, impaired coordination, and sensory deficits, affecting the ability to maintain a stable stance.
Finally, musculoskeletal factors, such as joint pain, muscle tightness, and limited range of motion, can also contribute to poor SLS performance. These factors can restrict movement and reduce stability, making it challenging to maintain a balanced stance for an extended period.

